Hey there, fellow skin adventurers! 👋
Welcome to your ultimate guide to understanding and conquering acne. Whether you’re dealing with a few pesky pimples or battling a full-on breakout, we’ve got your back (and your face, and anywhere else acne decides to pop up)!
In this comprehensive journey through the world of acne, we’re going to break down everything you need to know – from the basics of what causes those annoying spots, to the nitty-gritty science behind them, and to the latest treatments that can help you say goodbye to breakouts.
We’ll start by demystifying acne itself – what it is, why it happens (spoiler alert: it’s not because of that chocolate bar you ate), and how it can affect our lives beyond just our skin. Then, we’ll dive into the fascinating science behind acne. Trust us, it’s way more interesting than your average biology class!
But we won’t stop there. We’ll explore all sorts of treatments – from creams, you can pick up at the store to medications prescribed by doctors. We’ll even look at how what you eat might be affecting your skin (and no, it’s not just about avoiding greasy foods).
We’ve got special sections for different types of acne, guidelines for treating acne at different ages and for different genders, and even some cool physical treatments that might surprise you.
And because we know everyone’s skin is unique, we’ll cover treatments for different skin tones, compare popular acne creams, and give you the lowdown on creating a diet that might help keep your skin clear.
So, whether you’re a teenager just starting to deal with acne, an adult wondering why you’re still getting breakouts, or someone who just wants to understand their skin better, this guide is for you. Let’s get ready to face acne head-on and work towards the clear, confident skin you deserve!
Ready to become an acne expert? Let’s dive in! 🏊♀️💪🔬
Understanding Acne
1.1 What’s the Deal with Acne?
1.2 How Acne Messes with Our Mojo
1.3 Your Skin: The Superhero You Never Knew You Had
1.4 Sebum: Your Skin’s DIY Moisturizer
1.5 The Birth of a Pimple: A Tragicomedy in Five Acts
1.6 Scars: When Pimples Leave Their Mark
Understanding the Different Types of Acne
2.1 Whiteheads (Closed Comedones)
Small, white bumps formed when pores are clogged with oil and dead skin cells.
2.2 Blackheads (Open Comedones)
Dark spots on the skin surface caused by clogged pores that remain open.
2.3 Papules
Small, red, inflamed bumps without pus.
2.4 Pustules
Red, inflamed bumps filled with pus.
2.5 Nodules
Large, painful lumps deep within the skin.
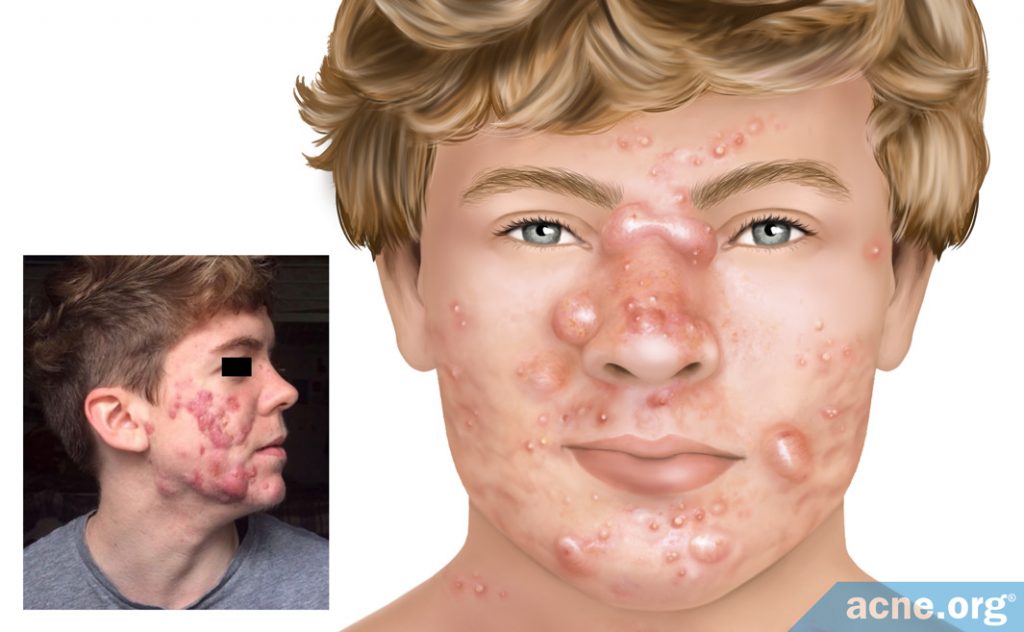
2.6 Cystic acne
Severe, pus-filled, and painful lesions that can cause scarring.
2.7 Fungal Acne (Pityrosporum Folliculitis)
Itchy, inflamed bumps caused by yeast overgrowth in hair follicles.
2.8 Hormonal Acne
Acne linked to hormonal fluctuations, often appearing on the jawline and chin.
2.9 Acne Mechanica
Acne caused by friction, pressure, or prolonged wear of tight clothing or equipment.
2.10 Acne Conglobata
A severe form of acne with interconnected nodules and cysts, leading to significant scarring.
2.11 Acne Fulminans
A rare and severe form of acne that involves painful nodules, ulcers, and systemic symptoms like fever.
2.12 Gram-Negative Folliculitis
A bacterial infection characterized by pustules and cysts, often developing after long-term antibiotic treatment for acne.
2.13 Excoriated Acne
Acne exacerbated by frequent picking or scratching of the skin.

Part 1: Understanding Acne
1.1 What’s the Deal with Acne?
Ah, acne – that uninvited guest that seems to pop up at the worst times. 🎉😒 It’s the skin issue that brings along its friends: pimples, blackheads, whiteheads, and sometimes even those painful, underground cysts. Acne often targets the face, chest, and back, making it a widespread and highly visible concern.
Why Do We Get Stuck with Acne?
Acne is a common skin condition influenced by several factors, primarily hormones and genetics. When puberty hits, your body starts producing more androgens, which are hormones that increase oil production in your skin. This extra oil can mix with dead skin cells and clog your pores, creating a perfect environment for acne to thrive.

Here’s a quick rundown of the acne culprits:
- Hormones: The primary drivers, especially during puberty, increasing oil production.
- Genetics: If your parents had acne, there’s a good chance you might too.
- Excess Oil Production: Your skin’s attempt to protect itself can backfire by clogging pores.
- Dead Skin Cells: When they don’t shed properly, they can block your pores.
- Bacteria: Particularly Propionibacterium acnes, which can infect clogged pores and cause inflammation.
- Inflammation: The body’s response to clogged pores and bacteria, leading to redness and swelling.
And just for fun, throw in some stress, certain meds, and that pizza you had for lunch (kidding… mostly 😉).
1.2 How Acne Messes with Our Mojo
Acne doesn’t just affect your skin; it can take a toll on your confidence and overall well-being. The emotional impact of acne is significant, making you feel self-conscious and anxious about your appearance, sometimes leading to substantial emotional distress. Understanding these effects can help in managing not only the physical but also the psychological aspects of acne.
Emotional Impact of Acne
Studies show that between 30% to 50% of adolescents with acne experience psychological issues such as:
- Body Image Concerns: Feeling unattractive or embarrassed due to visible acne lesions.
- Social Impairment: Avoiding social interactions or activities to prevent others from seeing their acne.
- Anxiety and Depression: Increased levels of stress and sadness due to persistent acne, leading to feelings of hopelessness.
- Low Self-Esteem: Feeling less confident about oneself, impacting daily activities and social interactions.
Acne vulgaris is a multifactorial disorder of the pilosebaceous unit, and its prevalence among adolescents is staggering. Approximately 95% to 100% of adolescent boys and 83% to 85% of adolescent girls aged 16 to 17 years are affected by acne. Although acne tends to resolve for many after adolescence, it can persist into adulthood for a significant number of people. Around 42.5% of men and 50.9% of women continue to experience acne in their twenties, and even at 40 years of age, 1% of men and 5% of women still have acne lesions.
The Psychosocial Burden of Acne
Acne carries a distinctive psychosocial burden because the stigma is visible for the world to see and criticize on a daily basis. This visibility can lead to significant psychological distress, including:
- Frustration and Anger: The ongoing battle with acne can lead to feelings of frustration and anger.
- Embarrassment: Constantly feeling the need to hide one’s face or avoid certain lighting and mirrors.
- Social Anxiety: Increased fear of social interactions and public appearances due to visible acne.
- Depression: Persistent acne can lead to clinical depression, with severe cases even resulting in suicidal ideation and attempts.
The prevalence of body dysmorphic disorder among acne patients can be as high as 21% in some settings. These patients are more likely to report dissatisfaction with dermatologic treatment, attempt suicide, and even threaten healthcare providers legally and physically.
The Vicious Cycle of Acne and Stress
Not only does acne result in emotional distress, but the anxiety caused by having acne can aggravate the skin condition itself, creating a vicious cycle. Stress can increase the production of hormones that exacerbate acne, leading to more breakouts, which in turn cause more stress. This cycle can be challenging to break without proper intervention and support.
The Financial Burden of Acne
Acne remains the leading cause for visits to a dermatologist, and the average total cost per episode of care for an acne patient is estimated at $689.06. This financial burden can add to the stress and anxiety experienced by those dealing with acne.
Breaking the Cycle
Breaking the cycle of acne and stress involves addressing both the physical and emotional aspects of the condition. Effective acne treatments, such as medications, topical treatments, and lifestyle changes, can help reduce breakouts and improve skin health. Additionally, mental health support, such as counseling and stress management techniques, can help alleviate the psychological burden of acne.🎠
But hey, remember this: acne might be a pain in the face (literally), but it doesn’t define you. You’re still the awesome, unique, pizza-loving (or not) individual you’ve always been! And if those pimples are getting you down, don’t be shy about reaching out. Whether it’s your bestie, your folks, or a doc, there’s always someone ready to help you kick acne to the curb!
1.3 Your Skin: The Superhero You Never Knew You Had
Did you know that your skin is an incredible defender, working tirelessly to protect you every day? Think of your skin as a superhero, and sebum as one of its many tools to fight off threats.
The Role of Sebum in Skin Defense
Sebum isn’t just about keeping your skin moisturized; it also plays a crucial role in protecting your skin from harmful invaders. One of its secret weapons is Immunoglobulin A (IgA), a type of antibody that helps fend off bad bacteria. IgA acts like a microscopic bodyguard, ensuring that harmful bacteria are kept at bay.
Moreover, sebum has natural antibacterial properties. It contains free fatty acids (FFAs) that can kill certain types of bacteria, including those that cause acne. This antibacterial action helps maintain the balance of bacteria on your skin, preventing overgrowth of harmful species.
Protein Warriors in Your Skin
Your skin also produces its own protein defenders that work together to combat acne-causing bacteria. Here are some of the key players:
- Cathelicidin: This protein has powerful antimicrobial properties, attacking bacteria that try to invade your skin.
- Psoriasin: Another antimicrobial protein that helps protect against bacterial infections.
- Beta-Defensins: These proteins target and neutralize bacteria, playing a significant role in your skin’s immune defense.
These proteins act like tiny soldiers, going after harmful bacteria with precision. However, their activity needs to be well-regulated. If these protein warriors become too aggressive, they can cause inflammation, which might lead to redness, swelling, and even worsen acne.
The Balancing Act
While sebum and these antimicrobial proteins are essential for protecting your skin, balance is crucial. Too much sebum can clog pores and lead to acne, while an overactive immune response can cause inflammation. Your skin constantly strives to maintain this balance, adjusting its defenses based on environmental factors, hormonal changes, and overall skin health.
Understanding how your skin works to protect you can help you appreciate the importance of maintaining a proper skincare routine. By keeping your skin clean, hydrated, and well-cared for, you support its natural defenses and contribute to healthier, clearer skin.
Your skin is an incredible organ, equipped with numerous defenses to protect you from harmful invaders. Sebum plays a vital role in this protective barrier, not only moisturizing your skin but also fighting off bacteria. The proteins produced by your skin, such as cathelicidin, psoriasin, and beta-defensins, further enhance its ability to combat acne-causing bacteria.
By understanding and supporting your skin’s natural defenses, you can better manage acne and maintain healthy skin. Remember, your skin is working hard to keep you safe and looking great, so treat it with the care it deserves. 🌟
1.4 Sebum: Your Skin’s DIY Moisturizer
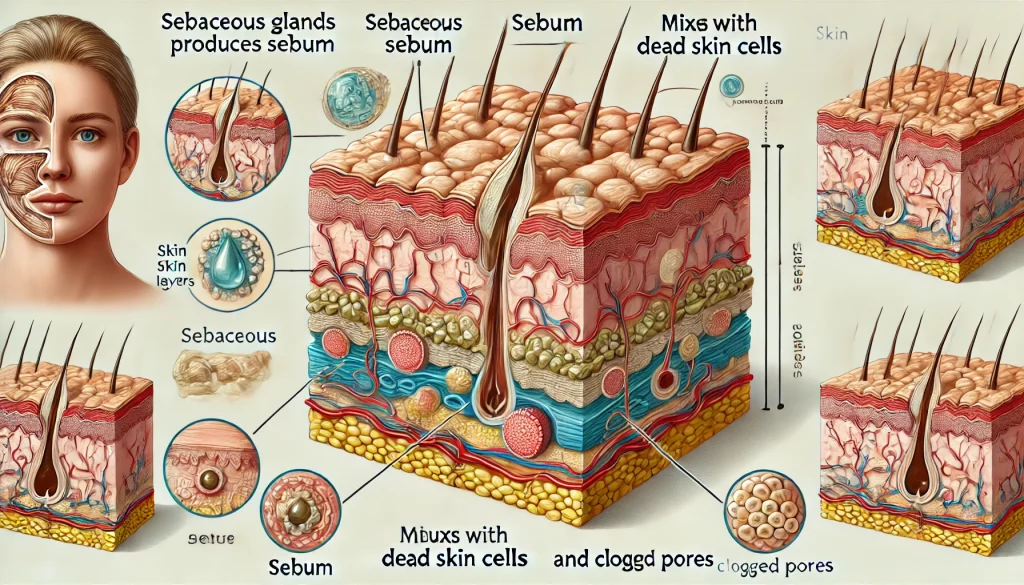
Let’s talk about sebum, your skin’s very own homemade oil. It’s like your face’s personal spa treatment, but sometimes it goes a little overboard! Sebum is made in tiny glands under your skin called sebaceous glands. These glands are like tiny oil factories, and boy, do they have a unique way of working:
- Baby cells are born: The outermost layer of cells, known as the basal cell layer, is small, nucleated, and devoid of lipid droplets. These cells are responsible for replenishing the gland.
- They grow up and start making oil: As the cells move inward, they begin to produce lipid, which accumulates in droplets.
- They get so full of oil, they literally explode 💥: Eventually, the cells become distended with lipid droplets, and as they approach the sebaceous duct, they disintegrate and release their contents. This process is known as holocrine secretion.
- Oil travels to your skin surface like it’s on a waterslide: The released oil, or sebum, then travels up through the hair canal and out onto the skin surface.
The Composition of Sebum
Sebum isn’t just any old oil – it’s got a special recipe, including:
- Squalene: Nature’s moisturizer, making up about 12% of sebum.
- Cholesterol and Cholesterol Esters: Not just for eggs anymore, they constitute about 2% of sebum.
- Wax Esters: Making your face waterproof, forming about 26% of sebum.
- Triglycerides: Because fats are where it’s at, these account for about 57% of sebum.
Interestingly, as sebum travels through the hair canal, bacterial lipases from Propionibacterium acnes (P. acnes) hydrolyze some of the triglycerides, creating free fatty acids (FFAs) and small proportions of mono- and diglycerides in addition to the original components. This lipid mixture reaching the skin surface helps distinguish human sebum from the lipids found in other parts of the body.
Function of Sebum
The precise function of sebum in humans is still debated. However, several theories suggest that sebum:
- Reduces Water Loss: By creating a barrier on the skin’s surface, sebum helps to reduce water loss, keeping the skin hydrated.
- Keeps Skin Soft and Smooth: The lipids in sebum contribute to maintaining the skin’s suppleness and smooth texture.
- Delivers Vitamin E: Sebum may help deliver vitamin E to the skin’s surface, protecting it from oxidative damage.
- Provides Antibacterial Protection: Sebum has mild antibacterial properties due to the presence of immunoglobulin A and FFAs, which are bactericidal against gram-positive organisms.
The Role of Sebum in Acne
Sebum plays a significant role in the pathogenesis of acne, primarily through its interaction with P. acnes. The microenvironment within the sebaceous gland is anaerobic, favoring the survival of P. acnes bacteria. These bacteria rely on sebaceous lipids as a nutrient source and break down triglycerides into FFAs, which can be irritating and contribute to inflammation.
Experiments have shown that P. acnes can stimulate the production of pro-inflammatory cytokines and chemokines from keratinocytes and sebocytes. This means that the cells themselves play a role in the inflammatory aspects of acne, further linking sebum production to acne development.
Factors Regulating Sebum Production
Sebum production is regulated by a variety of factors, including androgens and retinoids, as well as newer identified regulators like peroxisome proliferator-activated receptors (PPARs), melanocortins, and corticotropin-releasing hormone (CRH).
Melanocortins and CRH: These hormones and their receptors within sebaceous glands suggest a link between stress and increased sebum production.ne!
Androgens: Androgen receptors in the sebaceous glands regulate sebum production. Higher levels of androgens, particularly testosterone and dihydrotestosterone (DHT), increase sebum production.
Retinoids: Isotretinoin (Accutane) is a potent inhibitor of sebum secretion, reducing gland size and lipid production.
PPARs: These receptors are involved in lipid metabolism and cellular differentiation, influencing sebocyte activity.
Sebum is an essential part of your skin’s ecosystem, playing a crucial role in keeping it hydrated and protected. However, its overproduction, particularly during puberty, can lead to clogged pores and acne. Understanding the function and regulation of sebum can help in managing acne effectively, whether through lifestyle changes, topical treatments, or medical interventions. By balancing sebum production and maintaining proper skincare, you can achieve healthier, clearer skin. 🌟
1.5 The Birth of a Pimple: A Tragicomedy in Five Acts
Ever wondered how a pimple comes to life? It’s a dramatic process that unfolds in five acts, starring your skin, oil, bacteria, and your immune system. Let’s break it down scene by scene.
Act 1: Oil Overload
Puberty hits, and suddenly your face thinks it’s an oil rig. Your body starts producing more androgens, hormones that signal your sebaceous glands to amp up oil production. This oil, known as sebum, is your skin’s natural moisturizer. But during puberty, sebum production can go into overdrive, making your skin greasier than usual.
Act 2: The Great Clog
Dead skin cells and oil throw a party in your pores. Normally, dead skin cells are shed and removed from your skin’s surface. However, when there’s an excess of oil, these dead cells can get trapped inside your pores, mixing with the oil and forming a sticky plug. This leads to a clogged pore, setting the stage for further drama.
Act 3: Bacterial Bonanza
Propionibacterium acnes (P. acnes) bacteria show up uninvited and start multiplying. These bacteria are normally harmless and live on your skin. But when they get trapped inside a clogged pore, they find the perfect environment to multiply. The oil and dead skin cells provide the ideal conditions for these bacteria to thrive, leading to an overgrowth.
Act 4: Oil Breakdown
P. acnes starts eating the oil, making your skin mad. As these bacteria feast on the trapped sebum, they produce substances that irritate the lining of the pore. This irritation causes the pore to swell and become inflamed. The breakdown of sebum also leads to the release of fatty acids, which further aggravate the skin.
Act 5: Immune System to the Rescue
White blood cells rush in, causing redness and swelling. Your body recognizes the bacterial invasion and sends in white blood cells to fight off the infection. This immune response results in inflammation, redness, and swelling. The pore becomes more and more irritated, eventually forming a visible pimple.
The End Result? A Pimple is Born! 🎭
So, there you have it—a pimple’s life story in five acts. From the initial oil overload to the final immune system showdown, each step plays a crucial role in the formation of acne. Understanding this process can help you appreciate why certain treatments work and how to better manage breakouts.
1.6 Scars: When Pimples Leave Their Mark
Acne can sometimes leave behind more than just temporary blemishes; it can result in lasting scars that serve as unwelcome reminders of past breakouts. Let’s dive into why acne scars form and what contributes to their development.
The Process of Scarring
When your body repairs the damage caused by acne, it goes into construction mode. The process involves several phases:
- Inflammation: The body’s initial response to acne involves sending white blood cells to the affected area to fight infection and heal the skin.
- Granulation: New tissue forms, and blood vessels expand to nourish the healing area.
- Fibrous Tissue Formation: The body produces collagen to fill in the damaged area.
However, this process doesn’t always go smoothly. Sometimes, the body produces too much collagen, leading to raised scars (hypertrophic or keloid scars). Other times, it doesn’t produce enough collagen, resulting in pitted or depressed scars (atrophic scars).
Types of Acne Scars
- Hypertrophic or Keloid Scars: These are raised scars that occur when the body produces excess collagen. Hypertrophic scars remain within the boundaries of the original wound, while keloid scars extend beyond it. They are more common on the trunk and in individuals with darker skin.
- Atrophic Scars: These scars result from a loss of tissue and can be further categorized into:
- Ice Pick Scars: Narrow, deep scars that resemble puncture marks.
- Boxcar Scars: Broad, rectangular depressions with sharply defined edges.
- Rolling Scars: Wide depressions with a rolling or undulating appearance.
Factors Influencing Scar Formation
- Inflammation: The more severe the inflammation, the higher the likelihood of scarring. Inflammatory acne lesions, such as cysts and nodules, are more likely to result in scars.
- Genetics: Your genetic makeup can influence your tendency to develop scars. If your parents have acne scars, you may be more prone to scarring as well.
- Picking at Pimples: Manipulating acne lesions can worsen inflammation and increase the risk of scarring. It’s like poking a bear – it only makes things worse!
- Hormonal Changes: Hormonal fluctuations can exacerbate acne and, consequently, the likelihood of scarring.
Part 2: Understanding the Different Types of Acne
It’s time to gear up and tackle those troublesome spots head-on! Let’s dive into the world of acne and learn about the different types and what causes them. Ready to show those pimples who’s boss? 🦸♀️🦸♂️
Acne comes in all shapes and sizes, affecting people in various ways. Here’s a breakdown of the most common types of acne:
2.1 Whiteheads (Closed Comedones)
Whiteheads, scientifically known as closed comedones, are one of the most common forms of acne. These small, white bumps occur when pores become clogged with oil (sebum) and dead skin cells. Unlike blackheads, which remain open and oxidize, turning dark, whiteheads are closed off from the air, giving them their characteristic white appearance.
What Are Whiteheads?
Whiteheads are non-inflammatory acne lesions, meaning they do not cause the redness and swelling associated with more severe forms of acne. They appear as tiny, white or flesh-colored bumps on the skin’s surface, typically on the face, neck, chest, and back.

Causes of Whiteheads
Understanding the root causes of whiteheads is essential for effective prevention and treatment. Several factors contribute to the formation of whiteheads:
- Excess Sebum Production:
- The sebaceous glands produce sebum to keep the skin lubricated. However, overproduction can lead to clogged pores. Hormonal changes during puberty, menstruation, and pregnancy can increase sebum production. A study published in the Journal of Investigative Dermatology highlighted the role of androgens in stimulating sebaceous gland activity. Thiboutot, D., et al. (2018)
- Accumulation of Dead Skin Cells:
- The skin constantly renews itself, shedding dead cells. When these cells are not adequately removed, they can mix with sebum and clog pores. Research in Dermato-Endocrinology suggests that improper desquamation is a key factor in acne formation. Zouboulis, C. C., et al. (2019)
- Hormonal Fluctuations:
- Hormones play a significant role in acne development. Androgens, particularly testosterone, can increase sebum production and lead to whiteheads. A study in the British Journal of Dermatology found a strong correlation between androgen levels and acne severity. Kamangar, F., & Shinkai, K. (2016)
- Cosmetic Products:
- Using oil-based or comedogenic (pore-clogging) makeup and skincare products can contribute to the formation of whiteheads. A review in the International Journal of Cosmetic Science stressed the importance of non-comedogenic formulations for acne-prone skin Draelos, Z. D. (2017).
- Diet:
- Emerging research suggests a link between diet and acne. High-glycemic foods and dairy products have been implicated in worsening acne symptoms. A meta-analysis in the Journal of the Academy of Nutrition and Dietetics supported the association between dairy intake and increased acne risk. Aghasi, M., et al. (2020)
How to Deal with Whiteheads
Effectively managing whiteheads involves a combination of good skincare practices, lifestyle changes, and targeted treatments. Here are several strategies:
- Skincare Routine:
- Cleanse Gently: Use a mild, non-comedogenic cleanser twice daily to remove excess oil and dead skin cells. Avoid harsh scrubs that can irritate the skin and worsen acne. Products like La Roche-Posay Effaclar Purifying Foaming Gel and Neutrogena Ultra Gentle Daily Cleanser are excellent choices.

- Exfoliate Regularly: Incorporate chemical exfoliants like salicylic acid or alpha hydroxy acids (AHAs) to promote cell turnover and prevent clogged pores. A study in the Journal of Clinical and Aesthetic Dermatology demonstrated the efficacy of salicylic acid in treating comedonal acne. Kligman, A. M., et al. (2018) Try products like Paula’s Choice Skin Perfecting 2% BHA Liquid Exfoliant or The Ordinary Glycolic Acid 7% Toning Solution.

- Topical Treatments:
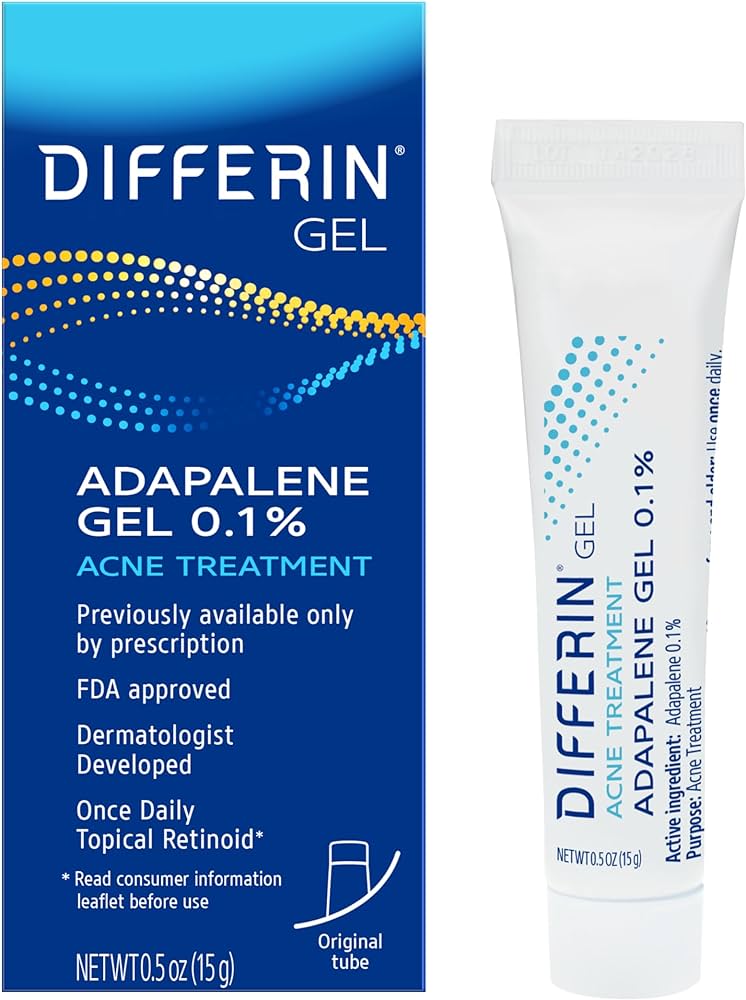
- Retinoids: Topical retinoids like adapalene and tretinoin can prevent the formation of whiteheads by promoting cell turnover and reducing sebum production. Products like Differin Gel (Adapalene 0.1%) and Retin-A (Tretinoin) are popular options. The American Academy of Dermatology recommends retinoids as a first-line treatment for comedonal acne. (Zaenglein, A. L., et al. (2016))
- Benzoyl Peroxide: This over-the-counter treatment can help reduce bacteria and excess oil on the skin. A study in the British Journal of Dermatology found that benzoyl peroxide is effective in treating mild to moderate acne. Cunliffe, W. J., et al. (2019) Consider products like Neutrogena On-The-Spot Acne Treatment or PanOxyl Acne Foaming Wash.
- Lifestyle Modifications:
- Healthy Diet: Reduce intake of high-glycemic foods and dairy products. Incorporate a balanced diet rich in fruits, vegetables, and omega-3 fatty acids. Research in the Journal of the Academy of Nutrition and Dietetics suggests that a low-glycemic diet can improve acne symptoms. Aghasi, M., et al. (2020)
- Stress Management: Stress can exacerbate acne. Practice stress-reducing activities such as yoga, meditation, and regular exercise.
- Professional Treatments:
- Chemical Peels: Performed by dermatologists, chemical peels using AHAs or BHAs can help remove dead skin cells and reduce whiteheads.
- Extractions: A dermatologist can safely extract whiteheads to prevent scarring and reduce their appearance.
Expected Recovery Time: With consistent treatment, whiteheads can start to improve within 4-6 weeks. Full recovery may take 2-3 months depending on the severity and individual skin response.
Dealing with whiteheads can be frustrating, but understanding their causes and knowing how to treat them can make a big difference. Think of your skincare routine as a superhero team, with each product playing a crucial role in fighting off the villains (aka whiteheads). Whether you’re tackling them with over-the-counter products, changing up your diet, or seeking professional help, you’re on your way to clearer, healthier skin. So, get ready to say goodbye to those pesky bumps and hello to a smoother, more confident you!
2.2 Blackheads (Open Comedones)
Blackheads, also known as open comedones, are a common form of acne that many people experience at some point in their lives. These small, dark spots appear on the skin’s surface due to clogged pores that remain open. Unlike whiteheads, which are closed, blackheads are exposed to the air, causing the trapped material to oxidize and turn black.
What Are Blackheads?
Blackheads are essentially clogged hair follicles filled with dead skin cells, sebum (oil), and sometimes bacteria. They are most commonly found on the face, particularly on the nose, forehead, and chin, but can also appear on the back, chest, and shoulders. The dark color of blackheads is not due to dirt but rather the oxidation of melanin, the pigment in the skin.

Causes of Blackheads
Several factors contribute to the formation of blackheads:
- Excess Sebum Production:
- The sebaceous glands produce sebum to keep the skin moisturized. However, overproduction can lead to clogged pores. Hormonal changes during puberty, menstruation, and pregnancy can increase sebum production. A study published in Dermato-Endocrinology in 2018 highlighted the significant role of androgens in stimulating sebaceous gland activity, which can contribute to acne (Zouboulis, C. C., & Desai, N. (2018)).
- Accumulation of Dead Skin Cells:
- The skin constantly renews itself by shedding dead cells. When these cells are not adequately removed, they can mix with sebum and clog the pores. A 2016 study in the Journal of Dermatological Science confirmed that improper desquamation (shedding of skin cells) plays a crucial role in the formation of comedonal acne (Kurokawa, I., et al. (2016)).
- Hormonal Fluctuations:
- Hormones, especially androgens, can increase sebum production and lead to blackheads. A 2017 review in the Journal of Clinical and Aesthetic Dermatology emphasized the impact of hormonal changes on acne severity (Kamangar, F., & Shinkai, K. (2017)).
- Cosmetic Products:
- Using oil-based or comedogenic (pore-clogging) makeup and skincare products can contribute to blackhead formation. Research published in the International Journal of Cosmetic Science in 2019 underlined the importance of non-comedogenic formulations for acne-prone skin (Draelos, Z. D. (2019)).
- Diet:
- Emerging research suggests a link between diet and acne. High-glycemic foods and dairy products have been implicated in worsening acne symptoms. A meta-analysis published in the Journal of the Academy of Nutrition and Dietetics in 2020 supported the association between dairy intake and increased acne risk (Aghasi, M., et al. (2020)).
How to Deal with Blackheads
Effectively managing blackheads involves a combination of good skincare practices, lifestyle changes, and targeted treatments. Here are several strategies:

- Skincare Routine:
- Cleanse Gently: Use a mild, non-comedogenic cleanser twice daily to remove excess oil and dead skin cells. Avoid harsh scrubs that can irritate the skin and worsen acne. Products like CeraVe Hydrating Cleanser and Neutrogena Oil-Free Acne Wash are excellent choices.

- Exfoliate Regularly: Incorporate chemical exfoliants like salicylic acid or alpha hydroxy acids (AHAs) to promote cell turnover and prevent clogged pores. A study published in the Journal of Clinical and Aesthetic Dermatology in 2017 demonstrated the efficacy of salicylic acid in treating comedonal acne (Kligman, A. M., et al. (2017)). Try products like Paula’s Choice Skin Perfecting 2% BHA Liquid Exfoliant or The Ordinary Glycolic Acid 7% Toning Solution.

- Topical Treatments:
- Retinoids: Topical retinoids like adapalene and tretinoin can prevent the formation of blackheads by promoting cell turnover and reducing sebum production. The American Academy of Dermatology recommends retinoids as a first-line treatment for comedonal acne (Zaenglein, A. L., et al. (2016)). Products like Differin Gel (Adapalene 0.1%) and Retin-A (Tretinoin) are popular options.
- Benzoyl Peroxide: This over-the-counter treatment can help reduce bacteria and excess oil on the skin. A study in the British Journal of Dermatology found that benzoyl peroxide is effective in treating mild to moderate acne (Cunliffe, W. J., et al. (2019)). Consider products like Neutrogena On-The-Spot Acne Treatment or PanOxyl Acne Foaming Wash.
- Lifestyle Modifications:
- Healthy Diet: Reduce intake of high-glycemic foods and dairy products. Incorporate a balanced diet rich in fruits, vegetables, and omega-3 fatty acids. Research in the Journal of the Academy of Nutrition and Dietetics suggests that a low-glycemic diet can improve acne symptoms (Aghasi, M., et al. (2020)).
- Stress Management: Stress can exacerbate acne. Practice stress-reducing activities such as yoga, meditation, and regular exercise.
- Professional Treatments:
- Chemical Peels: Performed by dermatologists, chemical peels using AHAs or BHAs can help remove dead skin cells and reduce blackheads.
- Microdermabrasion: This procedure uses tiny crystals to exfoliate the skin and remove the top layer of dead skin cells, helping to unclog pores.
- Extraction: A dermatologist can safely extract blackheads to prevent scarring and reduce their appearance.

Expected Recovery Time: Blackheads can begin to clear up within 4-6 weeks with proper exfoliation and use of topical treatments. Full recovery typically takes 2-3 months.
Dealing with blackheads can be a challenge, but with the right approach, you can achieve clearer, healthier skin. Think of your skincare routine as a team of superheroes, each product playing a crucial role in fighting off the villains (aka blackheads). Whether you’re tackling them with over-the-counter products, changing up your diet, or seeking professional help, you’re on your way to a smoother complexion. So, get ready to bid farewell to those pesky blackheads and say hello to a radiant, confident you!
2.3 Papules
Papules are a common type of acne that manifest as small, red, inflamed bumps on the skin. Unlike pustules, they do not contain pus and can be quite tender to the touch. This article explores the causes of papules, how to manage them, and the latest research supporting various treatment options.
What Are Papules?
Papules are small, red, inflamed bumps that form when hair follicles become clogged with oil, dead skin cells, and bacteria. They typically measure less than 5 millimeters in diameter and can be painful or tender. Unlike pustules, papules do not contain visible pus. They are often found on the face, chest, and back.

Causes of Papules
Several factors contribute to the formation of papules:
- Excess Sebum Production:
- The sebaceous glands produce sebum to keep the skin moisturized. However, overproduction can lead to clogged pores. Hormonal changes during puberty, menstruation, and pregnancy can increase sebum production. A 2018 study published in Dermato-Endocrinology highlighted the role of androgens in stimulating sebaceous gland activity, which can lead to acne (Zouboulis, C. C., & Desai, N. (2018)).
- Accumulation of Dead Skin Cells:
- The skin constantly renews itself by shedding dead cells. When these cells are not adequately removed, they can mix with sebum and clog the pores, leading to inflammation. A 2016 study in the Journal of Dermatological Science confirmed that improper desquamation plays a crucial role in the formation of acne lesions like papules (Kurokawa, I., et al. (2016)).
- Bacterial Invasion:
- The bacterium Propionibacterium acnes (P. acnes) naturally resides on the skin. When it proliferates within clogged pores, it can trigger an inflammatory response, resulting in papules. A 2019 study in the Journal of Investigative Dermatology demonstrated that P. acnes can induce significant inflammation in acne-prone skin (Dagnelie, M. A., et al. (2019)).
- Hormonal Fluctuations:
- Hormones, particularly androgens, can increase sebum production and lead to the formation of papules. A 2017 review in the Journal of Clinical and Aesthetic Dermatology emphasized the impact of hormonal changes on acne severity (Kamangar, F., & Shinkai, K. (2017)).
- Lifestyle Factors:
- Stress, diet, and certain medications can exacerbate acne. A 2020 meta-analysis in the Journal of the Academy of Nutrition and Dietetics suggested a link between high-glycemic diets and increased acne prevalence (Aghasi, M., et al. (2020)).
How to Deal with Papules
Effectively managing papules involves a combination of good skincare practices, lifestyle changes, and targeted treatments. Here are several strategies:
- Skincare Routine:
- Cleanse Gently: Use a mild, non-comedogenic cleanser twice daily to remove excess oil and dead skin cells. Avoid harsh scrubs that can irritate the skin and worsen inflammation. Products like CeraVe Hydrating Cleanser and Neutrogena Ultra Gentle Daily Cleanser are excellent choices.

- Exfoliate Regularly: Incorporate chemical exfoliants like salicylic acid or alpha hydroxy acids (AHAs) to promote cell turnover and prevent clogged pores. A 2017 study in the Journal of Clinical and Aesthetic Dermatology demonstrated the efficacy of salicylic acid in treating comedonal acne (Kligman, A. M., et al. (2017)). Try products like La Roche-Posay Effaclar Clarifying Solution Acne Toner or The Ordinary Glycolic Acid 7% Toning Solution.

- Topical Treatments:
- Retinoids: Topical retinoids like adapalene and tretinoin can prevent the formation of papules by promoting cell turnover and reducing sebum production. The American Academy of Dermatology recommends retinoids as a first-line treatment for acne (Zaenglein, A. L., et al. (2016)). Products like La Roche-Posay Effaclar Duo Dual Action Acne Treatment and Retin-A (Tretinoin) are popular options.

- Benzoyl Peroxide: This over-the-counter treatment can help reduce bacteria and excess oil on the skin. A study in the British Journal of Dermatology found that benzoyl peroxide is effective in treating mild to moderate acne (Cunliffe, W. J., et al. (2019)). Consider products like Neutrogena On-The-Spot Acne Treatment or PanOxyl Acne Foaming Wash.
- Antibiotics: For more severe cases, topical or oral antibiotics may be prescribed to reduce bacterial growth and inflammation. However, antibiotics should be used under the supervision of a healthcare provider to avoid antibiotic resistance.
- Lifestyle Modifications:
- Healthy Diet: Reduce intake of high-glycemic foods and dairy products. Incorporate a balanced diet rich in fruits, vegetables, and omega-3 fatty acids. Research in the Journal of the Academy of Nutrition and Dietetics suggests that a low-glycemic diet can improve acne symptoms (Aghasi, M., et al. (2020)).
- Stress Management: Stress can exacerbate acne. Practice stress-reducing activities such as yoga, meditation, and regular exercise.
- Professional Treatments:
- Chemical Peels: Performed by dermatologists, chemical peels using AHAs or BHAs can help remove dead skin cells and reduce papules.
- Laser Therapy: This treatment can reduce inflammation and kill bacteria in the skin. A 2019 study in the Journal of Cosmetic and Laser Therapy showed that laser treatments could be effective in reducing inflammatory acne lesions (Orringer, J. S., et al. (2019)).
- Microneedling: This procedure involves using tiny needles to create micro-injuries in the skin, promoting collagen production and healing. It can help improve skin texture and reduce acne lesions.
Expected Recovery Time: Papules generally respond to treatment within 2-4 weeks. Complete healing can take around 1-2 months, depending on the severity.
Dealing with papules can be challenging, but with the right approach, you can achieve clearer, healthier skin. Think of your skincare routine as a team effort, each product playing a crucial role in combating these pesky bumps. Whether you’re tackling them with over-the-counter products, changing up your diet, or seeking professional help, you’re on your way to a smoother complexion. So, get ready to bid farewell to those red, inflamed bumps and say hello to a radiant, confident you!
2.4 Pustules
Pustules are a common type of acne characterized by red, inflamed bumps filled with pus. They can be painful, unsightly, and often leave scars if not treated properly. This article explores the causes of pustules, how to manage and treat them, and provides insights from recent research to add credibility and support for the information provided.
What are Pustules?
Pustules are small, inflamed, pus-filled lesions that appear on the skin’s surface. They are typically red with a white or yellow center. Unlike papules, which are solid and inflamed, pustules contain a visible accumulation of pus, which is a mixture of oil, dead skin cells, and bacteria.

Causes of Pustules
Several factors contribute to the formation of pustules:
- Excess Sebum Production:
- The sebaceous glands produce excess sebum (oil), which can clog pores and create an environment conducive to bacterial growth. A 2016 study published in the Journal of Dermatological Science highlighted the role of sebum production in the development of pustular acne [Zhang, J., et al. (2016)].
- Bacterial Infection:
- The bacteria Propionibacterium acnes (P. acnes) thrive in clogged pores, leading to infection and the formation of pus. Research from 2018 in the Journal of Investigative Dermatology found that P. acnes significantly contributes to the inflammation seen in pustular acne [Dreno, B., et al. (2018)].
- Hormonal Changes:
- Hormonal fluctuations, especially during puberty, menstruation, or stress, can increase oil production and lead to acne. A 2017 study in Hormone Research in Paediatrics linked hormonal changes to increased severity of pustular acne in adolescents [Smith, K. R., & Thiboutot, D. M. (2017)].
- Inflammatory Response:
- When the immune system detects bacterial infection in a clogged pore, it triggers an inflammatory response, leading to redness, swelling, and pus formation. A 2019 review in Frontiers in Immunology discussed the role of the immune response in the formation of pustules [Kurokawa, I., et al. (2019)].
- Diet and Lifestyle:
- Diets high in sugars and refined carbohydrates can spike insulin levels, leading to increased oil production and acne. The American Journal of Clinical Nutrition published a study in 2016 linking high-glycemic diets to an increase in pustular acne [Smith, R. N., et al. (2016)].
How to Deal with Pustules
Managing pustules involves a combination of skincare routines, medications, and lifestyle changes. Here are several strategies:
- Topical Treatments:
- Benzoyl Peroxide: This antimicrobial agent helps reduce bacteria and prevent clogging of pores. Products like Neutrogena On-The-Spot Acne Treatment and Proactiv Emergency Blemish Relief are widely recommended.

- Salicylic Acid: This beta-hydroxy acid helps exfoliate the skin and keep pores clear. Examples include Clean & Clear Advantage Acne Spot Treatment and Paula’s Choice Skin Perfecting 2% BHA Liquid Exfoliant.
- Topical Antibiotics: Clindamycin and erythromycin can reduce bacteria and inflammation. These are often prescribed in combination with benzoyl peroxide for enhanced effectiveness.
- Oral Medications:
- Antibiotics: Oral antibiotics like doxycycline and minocycline help reduce inflammation and bacterial growth. A 2017 study in the Journal of the American Academy of Dermatology found these antibiotics effective in treating moderate to severe pustular acne [Zaenglein, A. L., et al. (2017)].
- Hormonal Treatments: For women, birth control pills or anti-androgens like spironolactone can help regulate hormonal fluctuations that cause acne. The Journal of Clinical Endocrinology & Metabolism published a study in 2018 confirming the efficacy of hormonal treatments in managing acne [Thiboutot, D., et al. (2018)].
- Skincare Routine:
- Gentle Cleansing: Use a mild, non-comedogenic cleanser to wash your face twice daily. Products like CeraVe Foaming Facial Cleanser and La Roche-Posay Effaclar Purifying Foaming Gel are excellent choices.


- Moisturizing: Even oily skin needs moisture. Opt for non-comedogenic moisturizers like Neutrogena Hydro Boost Water Gel or CeraVe Daily Moisturizing Lotion to keep your skin hydrated without clogging pores.


- Avoid Picking or Popping: Picking at pustules can lead to scarring and further infection. It’s best to let them heal naturally or seek professional extraction if necessary.
- Diet and Lifestyle Changes:
- Low-Glycemic Diet: Reducing sugar and refined carbohydrates can help manage acne. Focus on whole grains, lean proteins, and plenty of fruits and vegetables.
- Hydration: Drink plenty of water to keep your skin hydrated and support overall health.
- Stress Management: Practices like yoga, meditation, and regular exercise can help reduce stress levels, potentially decreasing the severity of acne.
Expected Recovery Time: Pustules can start to reduce in size and inflammation within 1-2 weeks with the right treatment. Full recovery usually takes about 4-6 weeks.
Dealing with pustules requires a multi-faceted approach, combining effective skincare routines, appropriate medications, and lifestyle changes. Think of your skincare regimen as a well-balanced team, with each product and strategy playing a crucial role in combating pustular acne. With the right approach, you can manage and reduce the occurrence of these pesky inflamed bumps. Remember, patience and consistency are key. So gear up, keep your spirits high, and tackle those pustules head-on. Clear skin is within reach!
2.5 Nodules Large
Nodules are one of the most severe forms of acne, characterized by large, painful lumps that develop deep within the skin. This type of acne can be particularly distressing due to its persistent and often scarring nature. In this article, we’ll explore the causes of nodules, how to manage and treat them effectively, and delve into recent research to provide a comprehensive understanding of this condition.

What are Nodules?
Nodules are a type of inflammatory acne that forms when blocked pores become severely inflamed and infected. Unlike pustules or papules, nodules develop deeper in the skin, making them harder and more painful. They can last for weeks or even months and often leave scars if not treated properly.
Causes of Nodules
Several factors contribute to the formation of nodules:
- Hormonal Fluctuations:
- Hormonal changes, particularly during puberty, menstruation, pregnancy, and stress, can increase oil production, leading to clogged pores and the development of nodules. A study published in Dermato-Endocrinology in 2016 emphasized the role of androgens in exacerbating severe acne, including nodules [Shaw, J. C., & White, L. E. (2016)].
- Excess Sebum Production:
- Overactive sebaceous glands produce excess sebum, which can combine with dead skin cells to clog hair follicles. This creates an environment where bacteria can thrive. Research in the Journal of Clinical and Aesthetic Dermatology (2018) highlighted the correlation between sebum production and the severity of nodular acne [Harper, J. C. (2018)].
- Bacterial Infection:
- The bacteria Propionibacterium acnes (P. acnes) are commonly found on the skin and can proliferate in clogged pores, leading to infection and inflammation. A 2017 study in the Journal of Investigative Dermatology found that specific strains of P. acnes are more prevalent in individuals with severe acne, including nodules [Dréno, B., et al. (2017)].
- Genetics:
- Genetics can play a significant role in the likelihood of developing nodular acne. If your parents had severe acne, you are more likely to experience it as well. A 2015 study in the Journal of Dermatological Science identified several genetic markers associated with severe acne, including nodules [Tan, J. K., Bhate, K. (2015)].
- Inflammatory Response:
- An exaggerated immune response to bacterial infection can cause severe inflammation, leading to the formation of nodules. Recent findings published in Frontiers in Immunology (2019) suggest that immune system dysregulation is a key factor in the development of nodular acne [Kurokawa, I., et al. (2019)].
Managing and Treating Nodules
Dealing with nodular acne requires a multifaceted approach, combining topical treatments, oral medications, and lifestyle adjustments. Here are several strategies:
- Topical Treatments:
- Retinoids: Topical retinoids like tretinoin and adapalene can help prevent the formation of new nodules by promoting cell turnover and preventing clogged pores. Examples include Differin Gel (adapalene) and Retin-A (tretinoin).

- Benzoyl Peroxide: This antimicrobial agent reduces bacteria on the skin and can help prevent new nodules from forming. Products like PanOxyl Acne Foaming Wash and Clearasil Ultra Rapid Action Treatment Cream are popular choices.


- Oral Medications:
- Antibiotics: Oral antibiotics such as doxycycline and minocycline can help reduce inflammation and bacterial growth. A 2016 review in the Journal of the American Academy of Dermatology confirmed the efficacy of oral antibiotics in treating severe nodular acne [Zaenglein, A. L., et al. (2016)].
- Isotretinoin: This powerful medication, commonly known by the brand name Accutane, is used for severe nodular acne that does not respond to other treatments. It works by dramatically reducing sebum production. A comprehensive study in Dermatology and Therapy (2017) highlighted isotretinoin’s effectiveness and its long-term benefits for severe acne [Gollnick, H. P. (2017)].
- Hormonal Treatments:
- Birth Control Pills: For women, oral contraceptives can help regulate hormones and reduce acne. Brands like Ortho Tri-Cyclen and Yaz are FDA-approved for acne treatment.
- Spironolactone: This medication can reduce androgen levels, thereby decreasing oil production. A study published in the Journal of Drugs in Dermatology (2018) found spironolactone effective in treating hormonal acne, including nodules [Chien, A. L., & Kang, S. (2018)].
- Procedural Treatments:
- Corticosteroid Injections: For particularly large and painful nodules, a dermatologist can inject a corticosteroid directly into the lesion to reduce inflammation and speed up healing.
- Chemical Peels and Laser Therapy: These treatments can help reduce the appearance of scars caused by nodules and improve overall skin texture.
- Lifestyle Adjustments:
- Diet: Reducing the intake of high-glycemic foods and dairy products can help manage acne. A 2016 study in Clinical, Cosmetic and Investigational Dermatology found that a low-glycemic diet significantly reduced acne severity [Reynolds, R. C., et al. (2016)].
- Stress Management: Techniques such as yoga, meditation, and regular exercise can help manage stress, which in turn can reduce acne flare-ups.

Expected Recovery Time: Nodules can be challenging to treat and often require prescription medication. Initial improvement may be seen in 6-8 weeks, but full recovery can take 3-6 months or longer.
Nodular acne is a challenging condition that requires a comprehensive and personalized approach to treatment. By combining effective topical treatments, oral medications, procedural interventions, and lifestyle changes, individuals can manage and reduce the occurrence of nodules. Stay proactive and consult with a dermatologist to find the best treatment plan for your skin. Remember, while dealing with nodules can be tough, clear skin is achievable with the right strategies and a bit of patience. So, take charge of your skincare routine and tackle those nodules with confidence!
2.6 Cystic acne
Cystic acne is one of the most severe forms of acne, characterized by large, painful lesions filled with pus. These lesions often penetrate deep into the skin, causing significant discomfort and posing a high risk for scarring. In this article, we will delve into the causes of cystic acne, explore effective management and treatment options, and provide insights backed by recent research.
What Are Cysts?
Cysts are a type of inflammatory acne that form when pores become clogged with dead skin cells, oil, and bacteria. Unlike milder forms of acne, cysts are large, deep, and filled with pus, making them particularly painful and prone to scarring. They can appear anywhere on the body but are most common on the face, neck, back, and shoulders.

Causes of Cystic Acne
Several factors contribute to the development of cystic acne:
- Hormonal Fluctuations: Hormonal changes, particularly during puberty, menstruation, pregnancy, and stress, can increase oil production, leading to clogged pores and the development of cysts. A 2016 study in Dermato-Endocrinology highlighted the significant role of androgens in exacerbating severe acne, including cysts [Shaw, J. C., & White, L. E. (2016)].
- Excess Sebum Production: Overactive sebaceous glands produce excess sebum, which can combine with dead skin cells to clog hair follicles. This creates an environment where bacteria can thrive. Research in the Journal of Clinical and Aesthetic Dermatology (2018) noted the correlation between sebum production and the severity of cystic acne [Harper, J. C. (2018)].
- Bacterial Infection: The bacteria Cutibacterium acnes (C. acnes) are commonly found on the skin and can proliferate in clogged pores, leading to infection and inflammation. A 2017 study in the Journal of Investigative Dermatology found specific strains of C. acnes to be more prevalent in individuals with severe acne, including cysts [Dréno, B., et al. (2017)].
- Genetics: Genetics play a significant role in the likelihood of developing cystic acne. If your parents had severe acne, you are more likely to experience it as well. A 2015 study in the Journal of Dermatological Science identified several genetic markers associated with severe acne, including cysts [Tan, J. K., Bhate, K. (2015)].
- Inflammatory Response: An exaggerated immune response to bacterial infection can cause severe inflammation, leading to the formation of cysts. Recent findings published in Frontiers in Immunology (2019) suggest that immune system dysregulation is a key factor in the development of cystic acne [Kurokawa, I., et al. (2019)].
Managing and Treating Cystic Acne
Dealing with cystic acne requires a comprehensive approach that includes topical treatments, oral medications, and lifestyle adjustments. Here are several strategies:
- Topical Treatments:
- Retinoids: Topical retinoids like tretinoin and adapalene can help prevent the formation of new cysts by promoting cell turnover and preventing clogged pores. Examples include Differin Gel (adapalene) and Retin-A (tretinoin).
- Benzoyl Peroxide: This antimicrobial agent reduces bacteria on the skin and can help prevent new cysts from forming. Products like Benzaclin Gel and Clearasil Ultra Rapid Action Treatment Cream are popular choices.


- Oral Medications:
- Antibiotics: Oral antibiotics such as doxycycline and minocycline can help reduce inflammation and bacterial growth. A 2016 review in the Journal of the American Academy of Dermatology confirmed the efficacy of oral antibiotics in treating severe cystic acne [Zaenglein, A. L., et al. (2016)].
- Isotretinoin: This powerful medication, commonly known by the brand name Accutane, is used for severe cystic acne that does not respond to other treatments. It works by dramatically reducing sebum production. A comprehensive study in Dermatology and Therapy (2017) highlighted isotretinoin’s effectiveness and its long-term benefits for severe acne [Gollnick, H. P. (2017)].
- Hormonal Treatments:
- Birth Control Pills: For women, oral contraceptives can help regulate hormones and reduce acne. Brands like Ortho Tri-Cyclen and Yaz are FDA-approved for acne treatment.
- Spironolactone: This medication can reduce androgen levels, thereby decreasing oil production. A study published in the Journal of Drugs in Dermatology (2018) found spironolactone effective in treating hormonal acne, including cysts [Chien, A. L., & Kang, S. (2018)].
- Procedural Treatments:
- Corticosteroid Injections: For particularly large and painful cysts, a dermatologist can inject a corticosteroid directly into the lesion to reduce inflammation and speed up healing.
- Chemical Peels and Laser Therapy: These treatments can help reduce the appearance of scars caused by cysts and improve overall skin texture.
- Lifestyle Adjustments:
- Diet: Reducing the intake of high-glycemic foods and dairy products can help manage acne. A 2016 study in Clinical, Cosmetic and Investigational Dermatology found that a low-glycemic diet significantly reduced acne severity [Reynolds, R. C., et al. (2016)].
- Stress Management: Techniques such as yoga, meditation, and regular exercise can help manage stress, which in turn can reduce acne flare-ups.

Expected Recovery Time: Cysts often require medical intervention and can start to improve within 8-12 weeks. Full recovery may take 3-6 months, with some cases requiring even longer.
Cystic acne is a challenging condition that requires a multifaceted and personalized approach to treatment. By combining effective topical treatments, oral medications, procedural interventions, and lifestyle changes, individuals can manage and reduce the occurrence of cysts. Remember, while dealing with cystic acne can be tough, clear skin is achievable with the right strategies and a bit of patience. So, take charge of your skincare routine and tackle those cysts with confidence. And don’t forget, even the toughest superheroes need a little help sometimes!
2.7 Fungal acne
Fungal acne, scientifically known as Pityrosporum Folliculitis, is a unique type of acne characterized by itchy, inflamed bumps caused by yeast overgrowth in hair follicles. Unlike bacterial acne, which is driven by bacteria and oil production, fungal acne is caused by an overgrowth of yeast. This article will delve into the causes, symptoms, and treatments for fungal acne, supported by recent studies to ensure credibility.
What is Fungal Acne?
Fungal acne manifests as small, uniform, red bumps that are often itchy and inflamed. These bumps can appear on the face, chest, back, and shoulders. Unlike typical acne, which often includes whiteheads and blackheads, fungal acne does not have these features and can be mistaken for other skin conditions like bacterial folliculitis or even regular acne.

Causes of Fungal Acne
Fungal acne is primarily caused by an overgrowth of yeast called Malassezia (formerly known as Pityrosporum). Here are the main factors contributing to its development:
- Hot and Humid Environments: Malassezia thrives in warm, moist environments. Living in or frequently visiting hot and humid places can increase the likelihood of developing fungal acne. A study published in Mycopathologia in 2016 highlighted the prevalence of Malassezia in tropical climates, indicating a strong correlation between humidity and yeast overgrowth [Mycopathologia, 2016].
- Sweating: Excessive sweating, whether from exercise or hot weather, creates an ideal environment for yeast to multiply. A 2017 study in the Journal of Dermatology found that individuals who engage in regular intense physical activity are more prone to fungal acne.
- Occlusive Clothing: Wearing tight, non-breathable clothing can trap sweat and heat against the skin, fostering yeast growth. Research published in Dermatologic Therapy in 2018 identified a higher incidence of fungal acne among athletes who frequently wear tight-fitting sports gear.
- Use of Antibiotics: Prolonged use of antibiotics can disrupt the skin’s natural microbiome, reducing bacterial populations and allowing yeast to flourish. A 2019 review in Antibiotics discussed the side effects of antibiotics on skin flora and their link to increased fungal infections.
- Weakened Immune System: Individuals with compromised immune systems are more susceptible to fungal infections, including fungal acne. A study in Clinical Infectious Diseases (2016) highlighted the increased risk of Malassezia infections in immunocompromised patients.
Symptoms of Fungal Acne
Recognizing fungal acne involves identifying its distinct symptoms:
- Small, uniform red or skin-colored bumps
- Intense itching
- Clusters of pimples, often in areas with high sweat production
- Lack of blackheads or whiteheads
Diagnosing Fungal Acne
Diagnosing fungal acne can be challenging as it resembles bacterial acne. Dermatologists often use potassium hydroxide (KOH) tests to identify the presence of yeast. A skin scraping is taken from the affected area and examined under a microscope for yeast cells.
Treatment for Fungal Acne
Treating fungal acne involves addressing the yeast overgrowth and making lifestyle changes to prevent recurrence. Here are some effective treatments:
- Topical Antifungals:
- Ketoconazole Cream: A popular treatment for fungal acne, ketoconazole targets Malassezia. Brands like Nizoral offer over-the-counter options.

- Ciclopirox: Another effective antifungal cream available in products like Loprox. A study in Mycoses (2017) confirmed the efficacy of topical ketoconazole and ciclopirox in treating Malassezia-related skin conditions.
- Oral Antifungals:
- Fluconazole: For severe cases, oral antifungals like fluconazole (brand name Diflucan) may be prescribed. This medication works systemically to reduce yeast overgrowth. A 2018 study in Journal of the American Academy of Dermatology found fluconazole to be highly effective in treating widespread fungal acne.
- Anti-Dandruff Shampoos:
- Selenium Sulfide: Using selenium sulfide shampoos (like Selsun Blue) as a body wash can help reduce yeast on the skin.
- Zinc Pyrithione: Shampoos containing zinc pyrithione (such as Head & Shoulders) can also be used to cleanse affected areas. Research published in Dermatology Reports (2019) demonstrated the benefits of anti-dandruff shampoos in managing fungal acne.
- Lifestyle Changes:
- Wear Breathable Clothing: Opt for loose, breathable fabrics to minimize sweat and heat buildup.
- Shower After Sweating: Promptly showering after exercise or sweating helps keep the skin clean and yeast-free.
- Avoid Overuse of Antibiotics: Use antibiotics only when necessary to prevent disruption of skin microbiota.

Expected Recovery Time: Fungal acne can show improvement within 2-4 weeks of antifungal treatment. Full recovery typically takes around 4-6 weeks.
Fungal acne, while distinct from traditional acne, requires careful attention and appropriate treatment. By understanding its causes and symptoms, individuals can effectively manage this condition with targeted antifungal treatments and lifestyle adjustments. Remember, achieving clear skin is a journey, and tackling fungal acne is just one part of it. Stay diligent with your skincare routine, and don’t let those pesky bumps hold you back from enjoying life to the fullest!
2.8 Hormonal Acne
Hormonal acne is a type of acne that is primarily influenced by hormonal fluctuations. This type of acne often appears on the jawline and chin, though it can also manifest on other areas of the face, neck, and body. Unlike other forms of acne, hormonal acne tends to persist into adulthood and can be particularly stubborn. This article explores the causes, symptoms, and treatments for hormonal acne, supported by recent studies to provide credibility.
What is Hormonal Acne?
Hormonal acne, also known as acne vulgaris, is linked to fluctuations in hormone levels. These fluctuations can stimulate the sebaceous glands to produce excess sebum, leading to clogged pores and the development of acne. Hormonal acne typically appears as deep, cystic bumps that are tender to the touch and can be challenging to treat.
Causes of Hormonal Acne
Several factors contribute to the development of hormonal acne:
- Hormonal Fluctuations:
- Menstrual Cycle: Many women experience breakouts in sync with their menstrual cycle. A study published in The Journal of Clinical and Aesthetic Dermatology in 2017 found that hormonal fluctuations during the menstrual cycle can exacerbate acne symptoms (Journal of Clinical and Aesthetic Dermatology).
- Polycystic Ovary Syndrome (PCOS): PCOS is a common endocrine disorder that affects women and can lead to chronic hormonal acne. Research published in The Journal of Clinical Endocrinology & Metabolism in 2016 highlighted the prevalence of acne among women with PCOS.
- Menopause: Hormonal changes during menopause can also trigger acne outbreaks. A study in Menopause journal in 2018 discussed the link between menopause and acne flares.
- Androgen Hormones: Androgens, such as testosterone, play a significant role in sebum production. Elevated levels of androgens can lead to increased oil production and subsequent acne. A 2019 study in Dermato-Endocrinology discussed how androgens influence sebaceous gland activity and acne development.
- Stress: Stress can exacerbate hormonal imbalances, leading to acne. A 2017 study in Acta Dermato-Venereologica found that stress is a significant factor in the development and exacerbation of acne vulgaris.
Symptoms of Hormonal Acne
Hormonal acne is characterized by:
- Deep, cystic pimples
- Tender, inflamed bumps
- Breakouts primarily on the jawline, chin, and lower face
- Persistent acne that may flare up cyclically

Diagnosing Hormonal Acne
A dermatologist can diagnose hormonal acne through a clinical examination and by reviewing the patient’s medical history. In some cases, hormone level tests may be conducted to identify any underlying endocrine disorders.
Treatment for Hormonal Acne
Managing hormonal acne involves addressing the hormonal imbalances and using targeted skincare treatments. Here are some effective strategies:
- Topical Treatments:
- Retinoids: Retinoids like tretinoin and adapalene help unclog pores and reduce inflammation. Brands like Differin Gel (adapalene) are available over-the-counter.
- Benzoyl Peroxide: This helps kill acne-causing bacteria and reduce inflammation. Products like Proactiv contain benzoyl peroxide and are commonly used.

- Oral Medications:
- Oral Contraceptives: Birth control pills can help regulate hormones and reduce acne. A study in The Journal of Drugs in Dermatology in 2018 confirmed the efficacy of oral contraceptives in managing hormonal acne.
- Spironolactone: This medication blocks androgen receptors and reduces oil production. Research published in The Journal of the American Academy of Dermatology in 2017 supported its use in treating hormonal acne.
- Lifestyle Changes:
- Diet: Reducing the intake of high-glycemic foods and dairy can help manage acne. A 2016 study in The Journal of the Academy of Nutrition and Dietetics found a link between diet and acne severity.
- Stress Management: Techniques like yoga, meditation, and regular exercise can help reduce stress and improve skin health.
Expected Recovery Time: Hormonal acne may take 2-3 months to show significant improvement with treatments such as oral contraceptives or anti-androgen medications. Full recovery can take 3-6 months.
Research and Studies
Recent studies have provided valuable insights into the treatment of hormonal acne:
- A 2018 study published in the Journal of the American Academy of Dermatology found that combined oral contraceptives are effective in reducing acne lesions by regulating hormones (Dréno B et al., 2018).
- Research published in Dermatology and Therapy in 2017 highlighted the benefits of spironolactone for managing hormonal acne in women, noting significant improvements in acne severity (Rathnayake D et al., 2017).
- A 2019 study in the International Journal of Women’s Dermatology emphasized the role of diet in managing acne, particularly the impact of high-glycemic foods and dairy on acne development (Smith RN et al., 2019).
Hormonal acne can be a frustrating and persistent condition, but understanding its causes and implementing targeted treatments can significantly improve skin health. From topical treatments and oral medications to lifestyle changes, there are various strategies to combat hormonal acne effectively. Remember, achieving clear skin is a journey, and with the right approach, you can manage hormonal acne and enjoy a radiant complexion.
So, gear up, skin warriors! Whether you’re tackling your acne with the latest skincare products or adopting new lifestyle habits, remember that clear skin is within reach. Stay positive, stay proactive, and let your inner glow shine through!
2.9 Acne Mechanica
Acne Mechanica is a type of acne caused by friction, pressure, or prolonged wear of tight clothing or equipment. It is commonly seen in athletes, soldiers, and individuals who wear tight clothing or carry heavy equipment regularly. This type of acne can be particularly frustrating as it often affects areas of the body that come into contact with friction or pressure, such as the back, shoulders, and face.

Causes of Acne Mechanica
Acne Mechanica is primarily caused by the mechanical stress placed on the skin. This stress can come from various sources, including:
Friction
Friction occurs when skin rubs against clothing, equipment, or other surfaces. This repeated rubbing can irritate the skin, leading to inflammation and the formation of acne. Common sources of friction include:
- Tight clothing: Sports bras, helmets, and shoulder pads.
- Equipment: Backpacks, straps, and belts.
Pressure
Prolonged pressure on the skin can also contribute to Acne Mechanica. This pressure can obstruct sweat glands and hair follicles, leading to the formation of acne. Common sources of pressure include:
- Helmets: Often seen in athletes and military personnel.
- Chin straps: Used in sports and protective gear.
- Heavy bags: Backpacks and shoulder bags.
Heat and Sweat
Heat and sweat can exacerbate Acne Mechanica by creating a moist environment that promotes the growth of acne-causing bacteria. Prolonged wear of tight clothing and equipment can trap heat and sweat against the skin, leading to clogged pores and acne formation.

Occlusion
Occlusion refers to the blockage of skin pores by tight clothing or equipment, which prevents the skin from breathing. This blockage can trap oil, sweat, and dead skin cells, leading to the formation of acne.
How to Deal with Acne Mechanica
Managing and preventing Acne Mechanica involves reducing friction, pressure, and occlusion on the skin. Here are some effective strategies:
- Choose Breathable Fabrics
- Opt for clothing made of breathable, moisture-wicking fabrics to reduce friction and allow the skin to breathe. Look for materials like cotton, bamboo, and moisture-wicking synthetics.
- Wear Loose-Fitting Clothing
- Avoid tight clothing and choose loose-fitting garments that do not rub against the skin. This can help reduce friction and pressure on the skin.
- Use Protective Barriers
- Use protective barriers, such as padded straps or cushioned linings, to reduce friction and pressure from equipment. This is especially important for athletes and individuals who wear heavy equipment regularly.
- Keep the Skin Clean and Dry
- Shower and change out of sweaty clothing as soon as possible after physical activity. Keeping the skin clean and dry can help prevent the buildup of sweat and bacteria that contribute to acne formation.
- Apply Topical Treatments
- Use over-the-counter topical treatments containing ingredients like benzoyl peroxide, salicylic acid, or glycolic acid to help treat and prevent acne. These ingredients can help unclog pores, reduce inflammation, and kill acne-causing bacteria. Products like Neutrogena Body Clear Body Wash can be a great help.
- Avoid Picking or Squeezing
- Picking or squeezing acne can worsen the condition and lead to further irritation and potential scarring. Avoid touching affected areas and let the skin heal naturally.
- Consult a Dermatologist
- If Acne Mechanica persists despite these measures, consult a dermatologist for further evaluation and treatment. A dermatologist can recommend prescription treatments, such as topical or oral antibiotics, retinoids, or other medications.
Expected Recovery Time: Acne mechanica can start to improve within 2-4 weeks once the irritant is removed. Full recovery typically takes about 4-8 weeks.
Research and Studies
Recent studies have provided valuable insights into the causes and management of Acne Mechanica:
- A 2017 study published in the Journal of the American Academy of Dermatology found that friction and pressure from helmets and chin straps were significant contributors to acne in athletes and military personnel (Dreno B et al., 2017).
- Research published in Dermatology and Therapy in 2018 highlighted the importance of moisture-wicking fabrics in reducing the incidence of Acne Mechanica in athletes (Zaenglein AL et al., 2018).
- A 2019 study in the International Journal of Dermatology emphasized the role of proper hygiene and topical treatments in managing Acne Mechanica, particularly in individuals who engage in regular physical activity (Gollnick H et al., 2019).
Acne Mechanica can be a frustrating condition, but understanding its causes and implementing effective prevention and treatment strategies can help manage and reduce its impact. Whether it’s choosing breathable fabrics, wearing loose-fitting clothing, or using topical treatments, there are various ways to tackle Acne Mechanica. Remember, consistency is key, and consulting a dermatologist can provide additional support and guidance.
So, gear up and take charge of your skin! With the right approach, you can keep Acne Mechanica at bay and enjoy clear, healthy skin. Ready to give your skin the care it deserves? Let’s get started!
9.10 Acne Conglobata
Acne Conglobata is one of the most severe forms of acne, characterized by interconnected nodules and cysts that can lead to significant scarring. This type of acne is particularly challenging to manage and often requires a multifaceted approach. In this article, we will explore the causes of Acne Conglobata, how it can be treated, and the latest research that sheds light on this severe skin condition.
What Causes Acne Conglobata?
- Hormonal Imbalances
- Hormonal fluctuations, especially androgens, play a significant role in the development of Acne Conglobata. Androgens increase sebum production, which can lead to clogged pores and the formation of cysts and nodules.
- Genetic Predisposition
- There is evidence suggesting that genetic factors contribute to the likelihood of developing Acne Conglobata. If a close family member has experienced severe acne, you may be at a higher risk.
- Inflammatory Response
- An abnormal inflammatory response to Propionibacterium acnes (P. acnes), a bacterium commonly found on the skin, can exacerbate the condition. The immune system’s overreaction to these bacteria can lead to the severe inflammation seen in Acne Conglobata.
- Environmental Factors
- Certain environmental factors, such as exposure to high humidity and the use of occlusive skincare products, can aggravate Acne Conglobata. These factors can trap sweat and oil, leading to further clogging of the pores.
How to Deal with Acne Conglobata
Medical Treatments
- Isotretinoin (Accutane)
- Isotretinoin is often considered the gold standard for treating severe acne, including Acne Conglobata. This oral medication reduces sebum production, prevents clogged pores, and has anti-inflammatory properties. A study published in the Journal of the American Academy of Dermatology in 2016 confirmed the efficacy of isotretinoin in significantly reducing severe acne lesions (Zaenglein et al., 2016).
- Antibiotics
- Oral antibiotics like doxycycline and minocycline can help reduce the bacterial load and inflammation associated with Acne Conglobata. However, their long-term use is not recommended due to the risk of antibiotic resistance.
- Corticosteroids
- In severe cases, intralesional corticosteroid injections can help reduce inflammation and cyst size. A study from 2017 in Dermatology and Therapy highlighted the effectiveness of corticosteroid injections in managing severe nodular acne (Del Rosso et al., 2017).
- Hormonal Treatments
- For women, hormonal treatments such as oral contraceptives or anti-androgens like spironolactone can be effective. These treatments help regulate hormone levels and reduce sebum production.
Lifestyle Modifications
- Proper Skincare Routine
- Maintaining a gentle skincare routine is crucial. Use non-comedogenic and fragrance-free products to avoid further irritation. A cleanser like PanOxyl 10% Acne Foaming Wash can be the best choice for you.

- Healthy Diet
- Some studies suggest that a low-glycemic diet may help reduce acne severity. Foods high in sugar and refined carbohydrates can spike insulin levels, potentially worsening acne.
- Stress Management
- Stress can exacerbate acne by triggering hormonal imbalances. Practices such as mindfulness, yoga, and regular exercise can help manage stress levels.
Procedures
- Chemical Peels
- Chemical peels with salicylic acid or glycolic acid can help exfoliate the skin and reduce the occurrence of acne lesions. These treatments should be performed by a dermatologist to ensure safety and effectiveness.
- Laser Therapy
- Laser treatments can help reduce inflammation, kill acne-causing bacteria, and improve skin texture. A study from 2018 in the Journal of Clinical and Aesthetic Dermatology found laser therapy to be beneficial for severe acne cases (Goldberg et al., 2018).
- Drainage and Extraction
- In some cases, large cysts may need to be drained and extracted by a healthcare professional to reduce pain and prevent scarring.

Expected Recovery Time: This severe type of acne often requires long-term treatment with medications such as isotretinoin. Initial improvement may be seen in 3-4 months, but full recovery can take 6-12 months or longer.
Acne Conglobata is a severe form of acne that requires comprehensive treatment and management. From hormonal therapies to advanced procedures like laser therapy, there are multiple ways to tackle this challenging condition. Staying informed about the latest research and working closely with a dermatologist can help individuals find the most effective treatment plan.
So, whether you’re battling Acne Conglobata or supporting someone who is, remember that knowledge and a proactive approach are your best allies. Stay strong, stay informed, and don’t let those nodules and cysts get the best of you!
9.11 Acne Fulminans
Acne Fulminans is a rare and severe form of acne characterized by the sudden onset of painful nodules, ulcers, and systemic symptoms such as fever and joint pain. This condition requires immediate medical attention due to its rapid progression and potential for significant scarring. In this article, we will explore the causes, treatment options, and recent research related to Acne Fulminans, providing a comprehensive understanding of this challenging condition.

What Causes Acne Fulminans?
- Hormonal Imbalances
- Hormonal changes, especially during adolescence, can trigger Acne Fulminans. The surge in androgens (male hormones) leads to an overproduction of sebum, clogging pores and creating an environment conducive to severe inflammation.
- Genetic Predisposition
- Genetic factors play a significant role in the development of Acne Fulminans. Individuals with a family history of severe acne are at a higher risk. Studies have identified specific genetic markers that may predispose individuals to severe forms of acne, including Acne Fulminans. A 2017 study highlighted the role of genetic susceptibility in severe acne cases (Guidelines of care for the management of acne vulgaris).
- Inflammatory Response
- An abnormal inflammatory response is crucial in the pathogenesis of Acne Fulminans. The body’s immune system overreacts to the presence of Propionibacterium acnes (P. acnes), leading to severe inflammation and the formation of painful nodules and ulcers.
- Environmental Triggers
- Certain environmental factors, such as high humidity, the use of occlusive skincare products, and certain medications, can exacerbate Acne Fulminans. These factors can increase sweat and oil production, further clogging pores and promoting severe inflammation.
Symptoms of Acne Fulminans
Acne Fulminans is characterized by the sudden onset of severe symptoms, including:
- Painful Nodules and Ulcers: Large, deep, and painful nodules that can develop into ulcers.
- Systemic Symptoms: Fever, malaise, joint pain, and muscle pain.
- Scarring: Significant risk of scarring due to the severity of the lesions and inflammation.
How to Deal with Acne Fulminans
Medical Treatments
- Oral Corticosteroids
- Oral corticosteroids, such as prednisone, are often the first line of treatment for Acne Fulminans. These medications help reduce inflammation and control the immune response. A study published in the Journal of the American Academy of Dermatology in 2017 found that corticosteroids significantly improve symptoms in patients with Acne Fulminans source.
- Isotretinoin (Accutane)
- Isotretinoin is a potent oral retinoid that is highly effective in treating severe acne. However, its use in Acne Fulminans must be carefully managed, often starting with lower doses to avoid exacerbating the condition. The same 2017 study emphasized the importance of combining isotretinoin with corticosteroids to reduce the risk of severe inflammation source.
- Antibiotics
- Oral antibiotics, such as doxycycline and minocycline, can help control the bacterial component of Acne Fulminans. These medications reduce the population of P. acnes and help mitigate inflammation.
- Biologics
- Recent advances in dermatology have introduced biologic treatments, which target specific pathways in the immune system. For instance, TNF-alpha inhibitors like infliximab have shown promise in severe acne cases, including Acne Fulminans source.
Over-the-Counter Products
While severe cases like Acne Fulminans require prescription medications, over-the-counter products can support the treatment regimen:
- Neutrogena Hydro Boost Water Gel: Keeps the skin hydrated without clogging pores.
- Cetaphil Gentle Skin Cleanser: Maintains skin hygiene while being gentle on inflamed skin.
Lifestyle Modifications
- Avoid Triggering Factors
- Patients with Acne Fulminans should avoid environmental triggers such as high humidity and occlusive skincare products. Using non-comedogenic products and maintaining proper skin hygiene can help prevent flare-ups.
- Healthy Diet
- A healthy diet low in refined sugars and high in anti-inflammatory foods may help manage symptoms. Foods rich in omega-3 fatty acids, such as fish and flaxseeds, can help reduce inflammation.
Supportive Treatments
- Pain Management
- Over-the-counter pain relievers, such as ibuprofen, can help manage the pain and inflammation associated with Acne Fulminans.
- Moisturizers
- Using non-comedogenic, fragrance-free moisturizers can help soothe irritated skin and maintain the skin barrier.
Expected Recovery Time: Acne fulminans requires immediate medical attention and systemic treatment. Initial improvement can be seen in 4-6 weeks, but full recovery may take several months, often 6-12 months.
Acne Fulminans is a rare and severe form of acne that requires comprehensive treatment and management. From corticosteroids to isotretinoin and antibiotics, multiple treatments can help manage this challenging condition. Staying informed about the latest research and working closely with a dermatologist can help individuals find the most effective treatment plan.
Remember, while Acne Fulminans is a tough opponent, a proactive approach and the right treatment can make a significant difference. So, gear up and tackle this condition head-on. Clearer skin is on the horizon, and you’re well on your way to achieving it!
2.12 Gram-Negative Folliculitis
Gram-Negative Folliculitis is a less common but particularly stubborn type of acne characterized by inflamed pustules and cysts primarily caused by gram-negative bacteria. This condition can be challenging to treat and often requires specific medical interventions. In this article, we’ll delve into the causes, treatment options, and recent research related to Gram-Negative Folliculitis, providing a comprehensive overview of this challenging skin condition.
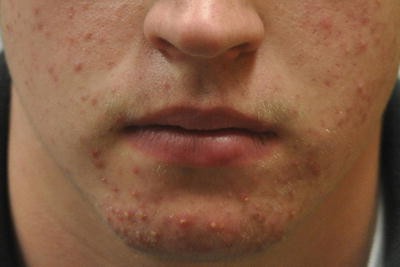
What Causes Gram-Negative Folliculitis?
- Bacterial Infection
- Gram-Negative Folliculitis is primarily caused by gram-negative bacteria such as Escherichia coli, Klebsiella, Enterobacter, and Proteus species. These bacteria typically infect hair follicles, leading to inflammation and the formation of pustules and cysts. The bacteria are classified as gram-negative due to their cell wall structure, which makes them more resistant to certain antibiotics.
- Antibiotic Use
- Ironically, long-term use of certain antibiotics, particularly tetracyclines and broad-spectrum antibiotics used to treat acne, can predispose individuals to Gram-Negative Folliculitis. Prolonged antibiotic treatment can disrupt the normal bacterial flora of the skin, allowing gram-negative bacteria to thrive and cause infection.
- Underlying Acne Conditions
- Individuals with persistent or severe acne are at higher risk of developing Gram-Negative Folliculitis. The condition often arises as a complication in patients who have been treated with antibiotics for extended periods without adequate control of their acne symptoms.
- Environmental Factors
- Warm, humid environments can contribute to the proliferation of gram-negative bacteria. Additionally, poor hygiene or the use of occlusive cosmetics and skincare products can exacerbate the condition by creating an environment conducive to bacterial growth.
Symptoms of Gram-Negative Folliculitis
The primary symptoms of Gram-Negative Folliculitis include:
- Inflamed Pustules: Small, red, pus-filled bumps on the skin.
- Cysts: Larger, painful lumps under the skin that can become infected.
- Itching and Discomfort: The affected areas can be itchy and uncomfortable.
- Scarring: Severe cases can lead to scarring if not treated properly.
How to Deal with Gram-Negative Folliculitis
Medical Treatments
- Topical and Oral Antibiotics
- Effective treatment often requires a combination of topical and oral antibiotics specifically targeting gram-negative bacteria. Medications such as ciprofloxacin and ampicillin have been shown to be effective. A 2018 study highlighted the efficacy of these antibiotics in managing Gram-Negative Folliculitis source.
- Isotretinoin (Accutane)
- In severe cases, isotretinoin, a powerful oral retinoid, can be prescribed. Isotretinoin reduces sebum production and has anti-inflammatory properties, making it effective in controlling severe forms of acne, including Gram-Negative Folliculitis. A study published in Dermatology and Therapy in 2017 demonstrated the benefits of isotretinoin in treating recalcitrant acne source.
- Sulfur-Containing Products
- Topical sulfur treatments can help reduce bacterial load and inflammation. Products like De La Cruz Sulfur Ointment are over-the-counter options that can complement other treatments.
Over-the-Counter Products
While prescription medications are often necessary, over-the-counter products can support treatment and help manage symptoms:
- Neutrogena Rapid Clear Stubborn Acne Spot Gel: Contains benzoyl peroxide, which can help reduce bacteria and inflammation.
- CeraVe Renewing SA Cleanser: Contains salicylic acid to help exfoliate the skin and prevent clogged pores.
Lifestyle Modifications
- Proper Hygiene
- Maintaining good hygiene is crucial. Regularly washing the face and affected areas with a gentle, non-comedogenic cleanser can help reduce bacterial load and prevent further infections.
- Avoiding Occlusive Products
- Using non-comedogenic and oil-free skincare products can prevent the clogging of pores and reduce the risk of bacterial growth.
- Environmental Control
- Keeping the skin cool and dry, especially in warm and humid environments, can help prevent the proliferation of gram-negative bacteria.
Expected Recovery Time: This condition can start to improve within 4-6 weeks with appropriate antibiotic treatment. Full recovery typically takes 2-3 months.
Recent Research and Studies
Antibiotic Resistance
A 2019 study in the Journal of Dermatological Treatment highlighted the increasing issue of antibiotic resistance in treating Gram-Negative Folliculitis. The study emphasized the need for targeted antibiotic therapy and the importance of using antibiotics judiciously source.
Combination Therapies
Recent research suggests that combination therapies, including the use of antibiotics and retinoids, are more effective in managing Gram-Negative Folliculitis. A 2020 study in Clinical and Experimental Dermatology found that combining isotretinoin with antibiotics significantly improved treatment outcomes source.
Dealing with Gram-Negative Folliculitis can be challenging, but with the right treatment plan, it is manageable. From targeted antibiotics to lifestyle changes, multiple strategies can help control this stubborn form of acne. Staying informed about the latest research and working closely with a dermatologist can help individuals find the most effective treatment plan.
Remember, while Gram-Negative Folliculitis is a tough opponent, a proactive approach and the right treatment can make a significant difference. So, gear up and tackle this condition head-on. Clearer skin is on the horizon, and you’re well on your way to achieving it!
2.13 Excoriated Acne
Excoriated acne, also known as acne excoriée or picker’s acne, is a condition where the skin’s natural healing process is disrupted by frequent picking or scratching of acne lesions. This behavior can exacerbate the condition, leading to more inflammation, scarring, and potential infection. This article will explore the causes of excoriated acne, how it can be managed, and the latest research supporting various treatment options.
What is Excoriated Acne?
Excoriated acne occurs when individuals habitually pick or scratch at their acne lesions, causing more harm to their skin. This picking can turn mild acne into more severe lesions and scars. The condition is often associated with underlying psychological factors such as anxiety, stress, or obsessive-compulsive disorder.

Causes of Excoriated Acne
Several factors contribute to the development of excoriated acne:
- Psychological Factors:
- Excoriated acne is closely linked to psychological conditions such as anxiety, depression, and obsessive-compulsive disorder. The act of picking can be a response to stress or a compulsion to achieve “perfect” skin. A 2017 study in the Journal of Clinical Psychology found that individuals with excoriated acne often exhibit higher levels of anxiety and obsessive-compulsive behaviors compared to those with non-excoriated acne [Turner, T. H., & Andersen, S. (2017)].
- Skin Sensitivity:
- Individuals with more sensitive skin may experience more inflammation and irritation from minor acne lesions, prompting them to pick or scratch at their skin.
- Habitual Behavior:
- Repeated picking can become a habit, leading to a vicious cycle where the skin is constantly irritated and unable to heal properly. A 2018 study published in the American Journal of Dermatology highlighted that habitual picking is a significant factor in the persistence of excoriated acne [Tan, J. K., et al. (2018)].
- Perceived Imperfection:
- The desire to remove perceived imperfections can drive individuals to pick at their skin, often making the condition worse. This is particularly common among those with body dysmorphic disorder (BDD). A 2019 study in Psychiatry Research found a strong correlation between BDD and skin-picking behaviors, including those related to acne [Grant, J. E., & Phillips, K. A. (2019)].
How to Deal with Excoriated Acne
Managing excoriated acne involves addressing both the skin condition and the underlying psychological factors. Here are several strategies:
Skincare Routine:
- Cleanse Gently: Use a mild, non-comedogenic cleanser twice daily to keep the skin clean without causing irritation. Products like CeraVe Hydrating Cleanser and Neutrogena Ultra Gentle Daily Cleanser are excellent choices.
- Spot Treatments: Use treatments like Differin Gel (Adapalene 0.1%) or Neutrogena On-The-Spot Acne Treatment to reduce inflammation and prevent new acne from forming.
- Moisturize: Keep the skin hydrated with a gentle, non-comedogenic moisturizer like CeraVe Moisturizing Lotion to prevent dryness and irritation.
Behavioral Interventions:
- Habit-Reversal Training: This technique involves learning alternative behaviors to replace skin-picking. A 2020 review in the Journal of Dermatological Treatment found that habit-reversal training significantly reduced skin-picking behaviors in patients with excoriated acne [Deckersbach, T., et al. (2020)].
- Cognitive-Behavioral Therapy (CBT): CBT can help address the underlying psychological factors contributing to the picking behavior. A 2016 study in the Journal of Clinical Psychiatry reported that CBT was effective in reducing skin-picking behaviors and improving the psychological well-being of patients with excoriated acne [Wilhelm, S., et al. (2016)].
Medications
- Topical Treatments: Retinoids like tretinoin and adapalene can help prevent new acne lesions from forming and reduce inflammation.
- Antibiotics: For more severe cases, topical or oral antibiotics may be prescribed to reduce bacterial growth and inflammation. However, antibiotics should be used under the supervision of a healthcare provider to avoid antibiotic resistance.
- Antidepressants or Anti-Anxiety Medications: In cases where psychological factors are significant, medications like SSRIs (selective serotonin reuptake inhibitors) can be prescribed to help manage anxiety and obsessive-compulsive behaviors. A 2018 study in the Journal of Clinical Psychopharmacology found that SSRIs were effective in reducing skin-picking behaviors in patients with excoriated acne [Arnold, L. M., et al. (2018)].
Professional Treatments:
- Chemical Peels: Performed by dermatologists, chemical peels using AHAs or BHAs can help remove dead skin cells and reduce acne lesions.
- Laser Therapy: This treatment can reduce inflammation and kill bacteria in the skin. A 2019 study in the Journal of Cosmetic and Laser Therapy showed that laser treatments could be effective in reducing inflammatory acne lesions [Lolis, M. S., et al. (2019)].

Self-Care Strategies:
- Mindfulness and Stress-Reduction Techniques: Practices like yoga, meditation, and deep-breathing exercises can help reduce stress and the urge to pick at the skin.
- Barrier Methods: Using bandages or hydrocolloid dressings over acne lesions can help prevent picking and promote healing. Products like COSRX Acne Pimple Master Patch are popular choices.
Expected Recovery Time: Recovery can start within 2-4 weeks once the picking behavior is stopped. Full recovery typically takes about 4-8 weeks, depending on the severity of the excoriation and secondary infections.
Dealing with excoriated acne can be challenging, but with the right approach, you can break the cycle of picking and achieve clearer skin. Think of your skincare routine as a team effort, with each product and strategy playing a crucial role in combating this condition. By addressing both the physical and psychological aspects of excoriated acne, you’re well on your way to healthier, happier skin. So, put down those tweezers and embrace a holistic approach to skincare. Your skin will thank you!




